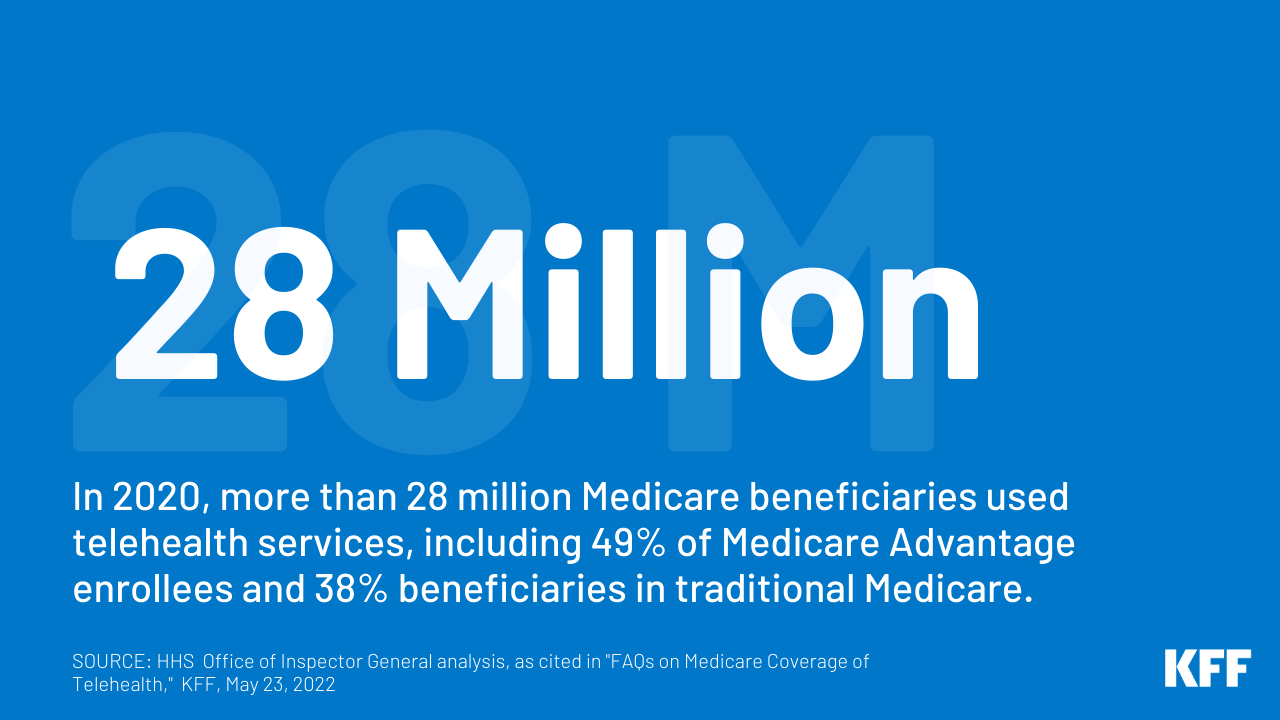
Telehealth, the supply of well being care companies to sufferers from suppliers who are usually not on the identical location, has skilled a fast escalation in use through the COVID-19 pandemic, amongst each privately-insured patients and Medicare beneficiaries. Previous to the pandemic, telehealth utilization amongst conventional Medicare beneficiaries was extremely low, with solely 0.3% of conventional Medicare beneficiaries enrolled in Half B utilizing telehealth companies in 2016. Between 2019 and 2020, the variety of telehealth visits in conventional Medicare elevated 63-fold. Through the first yr of the pandemic, more than 28 million Medicare beneficiaries general used telehealth companies, together with nearly half (49%) of Medicare Benefit enrollees and practically 4 in 10 (38%) beneficiaries in conventional Medicare.
These FAQs present solutions to questions on Medicare’s present protection of telehealth, modifications made on the outset of the general public well being emergency, extra modifications adopted by Congress and the Administration, and among the coverage concerns that lie forward.
What’s the present scope of Medicare telehealth protection and the way did it change at first of the COVID-19 pandemic?
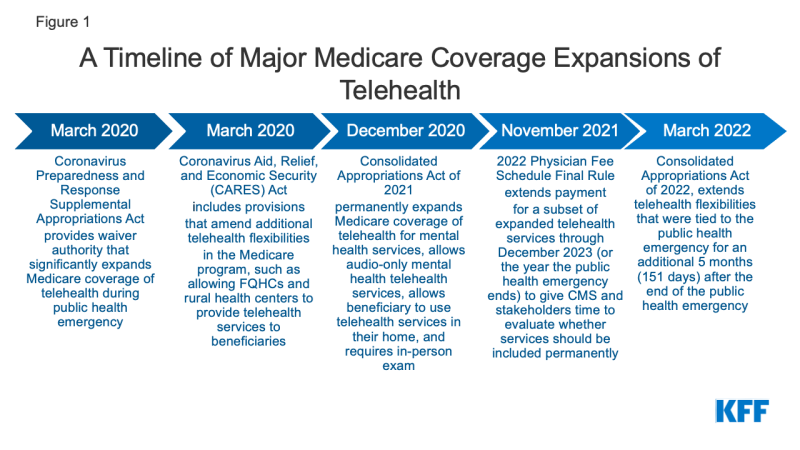
Beneath present regulation and rules, Medicare covers a broad scope of companies through telehealth with out restrictions that had been in place previous to the COVID-19 pandemic, however, for essentially the most half, this broader protection is obtainable solely briefly. Folks with Medicare can now entry telehealth companies, whether or not in city or rural areas, at residence or in different settings, utilizing audio-visual or audio-only applied sciences, and from a variety of well being care suppliers. This is because of a broad however time-limited enlargement of telehealth protection in Medicare through the COVID public well being emergency. To make it simpler and safer for beneficiaries to hunt medical care through the pandemic, in March 2020, the Secretary of the Division of well being and Human Providers (HHS) waived certain restrictions on Medicare coverage of telehealth services for Medicare beneficiaries through the COVID-19 public health emergency, based mostly on waiver authority included within the Coronavirus Preparedness and Response Supplemental Appropriations Act (and as amended by the CARES Act) (Determine 1). The general public well being emergency was most just lately renewed in April 2022, and the Biden Administration has stated that it’ll present a 60-day discover earlier than permitting the general public well being emergency to run out. As a result of the Biden Administration has not but offered a 60-day discover that the general public well being emergency will finish, it’s seemingly the PHE will lengthen past July.
The Consolidated Appropriations Act of 2022 (CAA of 2022) prolonged lots of the latest expansions of Medicare’s telehealth protection for roughly 5 months (151 days) after the top of the COVID-19 public well being emergency. This implies, for instance, if the general public well being emergency ends in October 2022, Medicare protection of telehealth would revert to extra restricted protection in March 2023, and most beneficiaries in conventional Medicare would lose entry to telehealth protection for many companies, aside from psychological well being companies (see beneath for extra data). It’s because earlier than the pandemic, protection of telehealth companies beneath Medicare was restricted to rural beneficiaries utilizing telehealth at an “originating web site,” akin to a clinic or physician’s workplace, moderately than from their very own properties. There have been additionally restrictions on which suppliers might be paid to ship telehealth companies (i.e., “distant web site” suppliers). There was additionally a comparatively restricted set of companies that might be lined by telehealth. (Medicare Benefit plans have flexibility to supply extra telehealth advantages past these which can be lined by conventional Medicare exterior of the general public well being emergency, as described beneath).
What companies can Medicare beneficiaries obtain by means of telehealth?
Earlier than the general public well being emergency, Medicare lined about 100 companies that might be administered by means of telehealth, together with workplace visits, psychotherapy, and preventive well being screenings, amongst different companies. Through the public well being emergency, the checklist of allowable telehealth services lined beneath Medicare has expanded to incorporate emergency division visits, bodily and occupational remedy, and sure different companies. Some analysis and administration, behavioral well being, and affected person schooling companies might be offered to sufferers through audio-only telephone.
Within the 2022 doctor price schedule final rule, the Facilities for Medicare & Medicaid Providers (CMS) briefly prolonged protection for a subset of the expanded telehealth companies by means of December 31, 2023 (or by means of the top of the yr wherein the general public well being emergency ends, whichever is later) to present each CMS and stakeholders time to judge whether or not they need to be completely included as Medicare-covered telehealth companies. These companies embrace bodily and occupational remedy, end-stage renal illness (ESRD) visits, emergency division visits, essential care companies, and others.
What psychological well being telehealth companies can be found for Medicare beneficiaries?
Telehealth has performed an essential position through the COVID-19 pandemic in offering entry to psychological well being companies for older adults, one in four of whom reported nervousness or melancholy in August 2020. Through the first yr of the pandemic, a big share of Medicare beneficiaries’ behavioral health services had been carried out through telehealth, and a bigger share of behavioral well being companies had been delivered through telehealth for beneficiaries in conventional Medicare (16%) than enrollees in Medicare Benefit (9%).
Based mostly on provisions within the Consolidated Appropriations Act of 2021, policymakers have completely expanded protection for telehealth companies for the aim of prognosis, analysis, or remedy of psychological well being issues after the top of the COVID-19 public well being emergency. Medicare beneficiaries can use telehealth for psychological well being companies of their properties, and beneficiaries who can not use real-time two-way audio and video for telehealth psychological well being companies are permitted to make use of audio-only gadgets to entry these companies. Beneficiaries are required to have an in-person, non-telehealth service inside six months of their first telehealth psychological well being service (though the CAA of 2022 delayed this requirement for 151 days after the top of the general public well being emergency).
What do Medicare beneficiaries pay for telehealth companies?
Beneficiary price sharing for telehealth companies has not modified through the public well being emergency. Medicare covers telehealth companies beneath Half B, so beneficiaries in conventional Medicare who use these advantages are topic to the Half B deductible of $233 in 2022 and 20% coinsurance. Nonetheless, the HHS Workplace of Inspector Common has provided flexibility for suppliers to scale back or waive price sharing for telehealth visits through the COVID-19 public well being emergency, though there aren’t any publicly-available information to point the extent to which suppliers might have achieved so. Most beneficiaries in conventional Medicare have supplemental insurance that will pay some or all the price sharing for lined telehealth companies. Medicare Benefit plans have flexibility to change cost-sharing necessities offered they meet requirements of actuarial equivalence and different CMS necessities.
What applied sciences can be utilized for telehealth companies?
Through the COVID-19 public well being emergency, telehealth companies lined by Medicare might be carried out through an interactive audio-video system, in addition to utilizing smartphones with real-time audio/video interactive capabilities with out different gear. Moreover, a restricted variety of telehealth companies might be offered to sufferers through audio-only telephone or a smartphone with out video (akin to phone analysis and administration companies and behavioral well being counseling).
When the 151-day interval after the general public well being emergency ends, a telehealth go to have to be carried out with two-way audio/video communications; the usage of audio-only telephones won’t be permitted, aside from psychological well being companies (as described above).
What kind of suppliers can get reimbursed by Medicare for telehealth companies?
Through the public well being emergency, any well being care skilled who’s eligible to invoice Medicare for skilled companies can present and invoice for telehealth companies and doesn’t must have beforehand handled the beneficiary. Additionally, federally certified well being facilities and rural well being clinics are eligible for reimbursement for telehealth companies offered to Medicare beneficiaries through the COVID-19 public well being emergency; these settings weren’t licensed as suppliers of telehealth companies for Medicare beneficiaries previous to statutory and regulatory modifications made originally of the pandemic.
If no different statutory modifications are made, as soon as the 151-day interval after the general public well being emergency ends, Medicare reimbursement for telehealth will revert to guidelines in place earlier than the general public well being emergency. Beneath these guidelines, solely physicians and sure different practitioners (akin to doctor assistants, medical social employees, and medical psychologists) will probably be eligible to obtain Medicare cost for telehealth companies offered to eligible beneficiaries in conventional Medicare, and so they will need to have handled the beneficiary receiving the companies within the final three years.
How does Medicare pay suppliers for telehealth companies?
Through the public well being emergency, Medicare pays for telehealth companies, together with these delivered through audio-only phone, as in the event that they had been administered in particular person, with the cost price various based mostly on the placement of the supplier, which implies that Medicare pays extra for a telehealth service offered by a physician in a non-facility setting, akin to a clinician’s workplace, than by a physician in a facility setting, akin to a hospital outpatient division. This additionally implies that through the public well being emergency, medical doctors in non-facility settings are receiving the next cost for companies offered by telehealth than they did earlier than the general public well being emergency.
Assuming no modifications to present regulation, Medicare’s cost for a telehealth service after the 151-day interval after the general public well being emergency ends would be the identical no matter whether or not it was offered in a non-facility setting or a facility setting, and the cost price will probably be based mostly on the decrease quantity paid to facility-based suppliers for a service delivered in particular person. (Beneath Medicare’s doctor price schedule, the cost to facility-based-providers for in-person companies is decrease than the cost to non-facility suppliers as a result of Medicare makes a separate cost to services to cowl apply bills, akin to bodily area, medical provides, medical gear, and medical workers time.) The rationale for utilizing the decrease facility cost quantity for telehealth companies is that apply bills for the supply of telehealth companies must be decrease than these for an in-person go to.
How do Medicare Benefit plans cowl telehealth?
Medicare Benefit plans are required to cowl all Half A and Half B advantages lined beneath conventional Medicare. Moreover, since 2020, Medicare Benefit plans have been capable of offer telehealth benefits not routinely lined by conventional Medicare (that’s, not through the COVID-19 public well being emergency), together with telehealth companies offered to enrollees in their very own properties and companies offered exterior of rural areas. In 2022, virtually all Medicare Advantage plans (98%) offer a telehealth benefit. Through the first yr of the COVID-19 pandemic, 49% of Medicare Benefit enrollees used telehealth companies.
Medicare Advantage plans are paid a capitated quantity by Medicare to offer primary Medicare advantages lined beneath Elements A and B, together with telehealth companies. Plans are actually permitted to incorporate prices related to extra telehealth advantages (past what conventional Medicare covers) of their bids for primary advantages.
Medicare Benefit plans have flexibility to waive sure necessities with regard to protection and price sharing in instances of catastrophe or emergency, such because the COVID-19 pandemic. CMS has advised plans that they might waive or scale back price sharing for telehealth companies, so long as plans do that uniformly for all similarly-situated enrollees. Many Medicare Benefit plans have waived or reduced cost sharing for enrollees for some or all companies administered through telehealth through the public well being emergency.
How is telehealth lined beneath Medicare for beneficiaries and suppliers collaborating in various cost fashions?
Like all different conventional Medicare beneficiaries, beneficiaries who obtain care by means of an alternate cost mannequin can entry expanded telehealth advantages through the public well being emergency. Separate from the time-limited expanded availability of telehealth companies, CMS has granted suppliers collaborating in some various funds fashions, together with Medicare Shared Financial savings Program ACOs, greater flexibility to provide care through telehealth, together with billing for telehealth companies offered to each city and rural beneficiaries and to beneficiaries when they’re at residence.
Will Medicare’s protection of “digital test ins” expire on the finish of the general public well being emergency?
Separate from Medicare’s protection of telehealth companies, Medicare covers temporary, “virtual check-ins” (additionally referred to as “temporary communication technology-based companies”) through phone or captured video picture, and E-visits for all beneficiaries, no matter whether or not they stay in a rural space. Each digital check-ins and E-visits, which had been out there to all beneficiaries previous to the general public well being emergency and can proceed to be out there to all beneficiaries after the general public well being emergency, are extra restricted in scope than a full telehealth go to. For instance, digital check-ins can solely be reported by suppliers with a longtime relationship to the affected person, can’t be associated to a latest medical go to (throughout the previous 7 days), and can’t result in a medical go to within the subsequent 24 hours (or the soonest out there appointment), and cost is meant to cowl solely 5-10 minutes of medical discussion.
What are present legislative proposals to increase Medicare protection of telehealth?
Policymakers are considering a wide range of proposals to increase some or all the current flexibilities surrounding telehealth companies beneath Medicare past the general public well being emergency, and many have expressed support for doing so. Among the many telehealth-related payments which have been launched within the 117th Congress are proposals to increase sure Medicare telehealth companies and to completely carry geographic and site-based restrictions for Medicare protection of telehealth. Different laws would permanently cover among the telehealth expansions offered through the public well being emergency and expand the scope of suppliers eligible for cost for telehealth companies lined by Medicare. Other bills are aimed toward assessing the impression of expanded telehealth companies in Medicare and Medicaid on utilization of telehealth visits, together with by demographics.
What coverage points are into account relating to the way forward for telehealth protection beneath Medicare?
Expanded protection of telehealth past the COVID-19 public well being emergency might have an effect on the standard of affected person care in addition to program and beneficiary spending. Broadening telehealth protection has the potential to improve access to wanted care, however the implications of telehealth for communities of coloration are usually not but clear, with analysis displaying each higher use in disadvantaged neighborhoods and lower use among black and rural Medicare beneficiaries than white beneficiaries. Furthermore, increasing telehealth protection would seemingly result in an general improve in Medicare program spending: CBO scored 5 months of expanded telehealth protection included within the CAA 2022 as costing $663 million. Nonetheless, some telehealth companies could also be substitutes for in-person care, akin to a behavioral well being care go to, although simpler entry to telehealth might result in an general improve in visits and prices. Different telehealth companies might not totally substitute the necessity for (or incidence of) an in-person go to, akin to when lab work is decided to be wanted.
Moreover, state licensing necessities might have an effect on entry to telehealth companies. Through the public well being emergency, states used emergency authority to waive facets of state licensing necessities for medical suppliers to make it simpler for folks to entry well being care through telehealth, and lots of of those waivers are ending. Greater than half of states have signed the Interstate Medical Licensure Compact, which creates an expedited pathway for state licensure for medical suppliers, though it doesn’t present reciprocity for suppliers who’ve a state license in a single state and need to apply in one other.
The potential enlargement of telehealth protection brings with it issues in regards to the potential for fraudulent activity. There have been several massive fraud cases involving telehealth corporations in recent times, most of which concerned the submission of fraudulent claims for gadgets, companies, and tests to Medicare and different insurers that had been by no means given or administered to sufferers. HHS’ Workplace of the Inspector Common (OIG) is conducting a number of research to evaluate the appropriateness of use of telehealth through the public well being emergency, together with an analysis of provider billing patterns with the intention to establish suppliers that might pose a danger for program integrity and an audit of telehealth services under Part B to guarantee that companies are assembly Medicare necessities. The Medicare Fee Advisory Fee (MedPAC) has really helpful that Medicare apply extra scrutiny to outlier clinicians who ship extra telehealth companies than others, in addition to requiring in-person visits earlier than clinicians can order high-cost gear or companies for beneficiaries.